1964 US Surgeon General's Report on Smoking
January 1964What Happened
US Surgeon General Luther Terry convened an advisory committee that issued a 387-page report concluding cigarette smoking causes lung cancer and chronic bronchitis. The report estimated average smokers had a nine- to ten-fold risk of lung cancer compared to non-smokers; heavy smokers faced at least twenty-fold risk. Hammond's Cancer Prevention Study I, tracking over one million Americans, provided key data.
Outcome
Congress required health warnings on cigarette packages by 1965. Television and radio cigarette advertising was banned by 1971.
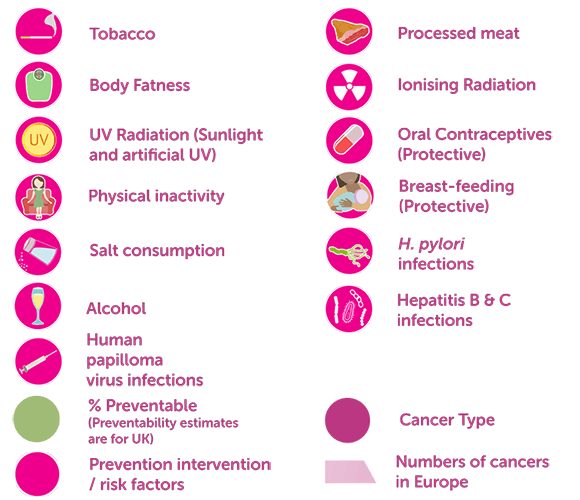
US adult smoking rates fell from 42% in 1964 to 11% by 2024. The report established the model for evidence-based public health policy that now informs global cancer prevention.
Why It's Relevant Today
The 2026 WHO/IARC analysis follows the same methodological approach—comprehensive data synthesis informing policy recommendations—that proved transformative for tobacco control.